Controlled Substance Diversion: Impact and Prevention
| ✅ Paper Type: Free Essay | ✅ Subject: Social Policy |
| ✅ Wordcount: 1889 words | ✅ Published: 18 May 2020 |
Abstract
Congress declared, “The illegal importation, manufacture, distribution, and possession and improper use of controlled substances [CSs] have a substantial and detrimental effect on the health and general welfare of the American people” (21 U.S.C § 801, 1970). CS abuse from 1999 to 2008 caused an increase of 300% of fatal opioid overdoses and contributed to over $72 billion annually that health insurers paid in health care expenses for opioid use (Larrat et al., 2014). The CDC attributes 78.1% of the 64,000 fatal overdoses in 2016 to opioid drugs obtained by CS diversion (CSD) and community sales (Kristof, 2018). Sadly, approximately 97.5 million people aged 12 and older in 2015 (36.4 percent of the American population) used CSs (Drug Diversion, 2017). Immediate action is needed to deter CSD and lower opioid abuse.
Background
In 1961, the United States (US) joined the Single Convention on Narcotic Drugs to institute mandates with regard to trafficking of CSs (21 U.S.C § 801, 1970). When President Nixon enacted the Controlled Substance Act (CSA) Title II of the Comprehensive Drug Abuse Prevention and Control Act of 1970, the Drug Enforcement Agency (DEA), the Department of Health and Human Services (HHS) and the Food and Drug Administration (FDA) initiated a “war on drugs” (Anderson 2012; Larrat et al., 2014). Almost fifty years later, the US suffers the highest drug use in history. One major contributing factor of this crisis is CSD in medical systems. Siegel (2019) stated that according to Title 21 of the US Code: CSs are “drugs classified as Schedule I through Schedule V by the FDA or applicable state law,” drug diversion is the “transfer of drugs from lawful to unlawful channels, such as a theft from hospital supply;” and theft is “when a person knowingly exerts unauthorized control over property and either (1) intends to deprive the owner of the property or (2) willingly and knowingly uses, conceals, or abandons the property in a way that actually deprives or will deprive the owner of the property.”
Analysis
Ten to fifteen percent of clinical workers in the US healthcare system will divert CSs in their careers, approximately 90% of which go undetected (American Society of Health-System Pharmacists [ASHP], 2017; Kristof, 2018; & Siegel, 2019). Carpenter (2014) cited research from 2001 identifying 10% of nurses “may be impaired or in recovery from alcohol or drug addiction.” CSD from hospitals increases disease outbreaks, drug-related hospitalizations, substance abuse admissions, overdose-related deaths and hospital risk (Kristof, 2018). Administrators, pharmaceutical management, protective services, nurse leadership and all hospital staff can collaborate to reverse this crisis by increasing awareness and prevention efforts, decreasing opportunities for diversion, enforcing corrective action, and assistance with prosecution of offenders.
CSD and abuse in hospitals primarily involves opioids, in part because they are the most prescribed pain medications (Siegel, 2019; Larrat et al., 2014). Federal hospitals are not exception, especially Veteran Affairs (VA) hospitals. More than 11,000 incidents of drug loss or theft were reported at federal hospitals between 2009 and 2016 as seen in figure 1, during which time the incidents rose from 272 in 2009 to 2,926 in 2015 (Yen, 2017). Between January 2014 and March 2016, federal hospitals reported about 92% of CSDs reported were lost in transit, 1.5% were theft, 1.2% were external theft, and 5.9% dispensing errors and other unknown reasons (Yen, 2017).
In 2010, excessive use of hydrocodone with acetaminophen for pain management and abuse were a result of 131.2 million prescriptions written (Carpenter, 2014). Patient harm, addicted health care workers (HCWs), HCWs’ dangerous activities around to other HCWs, loss of revenue and civil liability across health systems, as well as loss of life are all harmful results of CSD (Berge et al., 2012). “Hospitals bear the cost of diverted drugs, internal investigations and follow-up care for affected persons, and can be fined in excess of $4 million for inadequate safeguards” (Fan et al, 2019). The University of Michigan violation of the CSA (lack of DEA registrations and improper maintenance of records) resulted in a $4.3 million settlement, the largest CSA settlement of a hospital in history (Siegel, 2019).
Workplace overdoses from CSD rising at an almost unprecedented rate of more than 25% opioid-related mortality annually. Figures 2 and 3 shows the rise in fatal overdoses in the workplace increased 32% from 2015 to 2016 nationwide (Durden, 2017). Figure 4shows West Virginia, Ohio, Kentucky and Pennsylvania exceeding the national average (Durden, 2017). Figure 5 the demographic differences of opioid use in Ohio, most noticeably that males aged 25-54 experience the highest rates of addition and contributed to the most number of opioid-related overdose deaths in Ohio in 2015 (Durden, 2017).
To deter workers from consumption of CSs, health systems and other employers conduct drug screening during pre-employment and/or randomly during employment. Mieczkowski (1992) compared urine and hair mediums to determine the longevity of the presence of toxic substances. While CSs will generally remain in urine specimens for 3-5 days, the cortex of hair follicles will typically hold CSs for up to three months (figures 6 and 7) (Mieczkowski, 1992; Cuypers & Flanagan, 2018). “Hair analysis can be used for the determination of drug use months after drug consumption,” but is more expensive to process than urine or blood testing (Cuypers & Flanagan, 2018). Despite longer lasting traces of toxicity in hair, most employers still use urine and blood screening.
Innovation
State-mandated prescription medication programs (PMPs) provide health systems with best practices, policy initiatives and funding opportunities while developing national metrics (Larrat et al., 2014). To address concerns about utilization and patient care quality, legislation and regulations mandate that anyone who orders, handles, stores and distributes CS must register with the DEA, record inventories, maintain records and provide high-level security for all CSs (Larrat et al., 2014). Different states use different regulatory bodies to address compliance and PMPs (figure 8), such as Kentucky using a database access to move from 2nd to 31st in the nation for nonmedical use opioids (Larrat et al., 2014; Prescription Drug Monitoring Programs, 2017). Spending on drug enforcement more than doubled from 2009 to 2016 (figure 9) as the DEA, FDA and HHS struggled to prevent substance abuse nationwide (Becker, 2017). Figure 10 shows recent successes of government agencies combatting the opioid crisis (Siegel, 2019).
The Patient Protection and Affordable Care Act (ACA) requires health insurance providers to cover addiction treatment to increase accessible care for Americans. This innovative legislation helped states with expanded Medicaid to lower uninsured hospitalizations from CS abuse and mental health disorders by 15% between 2013 and 2015 (Kristof, 2018). Similar legislation has been enacted in some states, but nationwide policy regarding CSD is still limited.
Protective Services officers and security management play a significant role in preventing CSD by monitoring areas where pharmaceutical waste containers are located, surveilling cameras placed over CS entry/storage/use areas, and rounding on staff to reduce CSD (Kristof, 2018). Diversion monitoring software can also support surveillance activities (ASHP, 2017). Health technology specialist and innovators can contribute to making workplaces safer by working with government agencies and healthcare administrators on CSD prevention.
Policy Recommendation
It is necessary for healthcare administrators to cooperate with state and national agencies to lower CSD, protect healthcare workers and their patients, reduce economic waste, and defend health system integrity. Accomplishing this task will require PMPs to include:
- All staff who handle CSs to attend Employee Assistance Programs’ educational sessions annually, reviewing DEA forms 222, 41 & 106 (Carpenter, 2014; ASHP, 2017; Siegel, 2019),
- Random drug screening at least once every three months using hair analysis for every employee who handles CSs (Cuypers & Flanagan, 2018),
- Reports of all interactions with CS to supervising agencies (ASHP, 2017), and
- Surveillance programs that engage a multidisciplinary team to protect against document falsification, detection safeguards and drug tampering (Fan et al., 2019).
HCWs who are accountable for tampering with medications, theft, use and sale of CSs will perceive those negative actions to be more risky. By engaging HCWs in the PMP process, healthcare systems, state health departments and federal agencies can compile metrics to analyze, predict and prevent future CSDs.
Conclusion
Larrat et al. (2014) suggest, “The consequences of this diversion include adverse societal, clinical and economic impacts.” Too many lives being lost, resources stolen from hospitals and money being spent on CDS to survive the continued growth of the opioid crisis in the US. Costs of prevention and taking regulatory actions will be less than the billions of dollars spent/wasted from CSD and the incalculable value of lives lost. Legislative action must be taken to support the mandatory system-wide change that is needed to provide justification for action and funding.
References
- 21 U.S.C § 801 (1970). Retrieve from https://www.deadiversion.usdoj.gov/21cfr/21usc/801.htm
- American Society of Health-System Pharmacists [ASHP]. (2017). ASHP Guidelines on Preventing Diversion of Controlled Substances. American Journal of Health System Pharmacy, 74: 325-348. Retrieved from https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/preventing-diversion-of-controlled-substances.ashx
- Anderson, L. (2012, October 28). CSA Schedules. Retrieved from https://www.drugs.com/csa-schedule.html
- Becker, S. (2017, March 17). How Much Is the War on Drugs Really Costing Us? Retrieved from https://www.cheatsheet.com/money-career/financial-figures-americas-drug-war.html/
- Berge, K. H., Dillon, K. R., Sikkink, K. M., Taylor, T. K., & Lanier, W. L. (2012). Diversion of drugs within health care facilities, a multiple-victim crime: patterns of diversion, scope, consequences, detection, and prevention. Mayo Clinic proceedings, 87(7), 674–682. doi:10.1016/j.mayocp.2012.03.013
- Carpenter, H. (2014, December). The painful problem of drug diversion and what you can do. American Nurse Today, 9(12). Retrieved from https://www.americannursetoday.com/painful-problem-drug-diversion-can/?utm_source=BenchmarkEmail&utm_campaign=AMNT_Electronic_DEC14_House&utm_medium=email
- Cuypers, E., & Flanagan, R. J. (2018). The interpretation of hair analysis for drugs and drug metabolites. Clinical Toxicology (15563650), 56(2), 90–100. https://doi-org.ezproxy.umuc.edu/10.1080/15563650.2017.1379603
- Drug Diversion. (2017, May 29). Retrieved from https://www.premiersafetyinstitute.org/safety-topics-az/opioids/drug-diversion/
- Durden, T. (2017, December 31). The Opioid Crisis Invades The Workplace. Retrieved from https://www.zerohedge.com/news/2017-12-31/opioid-crisis-invades-workplace
- Fan, M., Tscheng, D., Hamilton, M., Hyland, B., Reding, R., Trbovich, P. (2019). Diversion of Controlled Drugs in Hospitals: A Scoping Review of Contributors and Safeguards. Journal of Hospital Medicine 7;419-428. doi:10.12788/jhm.3228
- Hair Follicle Drug Testing. (n.d.). Retrieved from https://www.dtpm.com/hair-testing/
- Kristof, T. (2018). Methods, Trends and Solutions of Drug Diversion (Evidence Based Healthcare Security Research Series, IAHSS Foundation). Retrieved from https://cdn.ymaws.com/www.iahss.org/resource/collection/48907176-3B11-4B24-A7C0-FF756143C7DE/2018_Methods,_Trends_and_Solutions_for_Drug_Diversion.pdf
- Larrat, E. P., Marcoux, R. M., & Vogenberg, F. R. (2014). Implications of recent controlled substance policy initiatives. P & T: a peer-reviewed journal for formulary management, 39(2), 126–128.
- Mieczkowski, T. (1992). New Approaches in Drug Testing: A Review of Hair Analysis. The Annals of the American Academy of Political and Social Science, 521, 132. Retrieved from https://search.ebscohost.com.ezproxy.umuc.edu/login.aspx?direct=true&db=edsjsr&AN=edsjsr.1046546&site=eds-live&scope=site
- Prescription Drug Monitoring Programs (PDMPs). (2017, February 22). Retrieved from https://www.usfhealthonline.com/resources/key-concepts/prescription-drug-monitoring-programs-pdmps/
- Siegel, M. (2019, July 30). Controlled Substances Diversion Training (2019 Edition): Holy Cross Germantown Hospital [PowerPoint slides].
- Yen, H. (2017, February 27). Low rate of discipline for drug loss and theft at VA hospitals, data shows. The Denver Post [Denver]. Retrieved from https://www.denverpost.com/2017/02/27/veterans-affairs-hospitals-opioid-theft/
Appendix
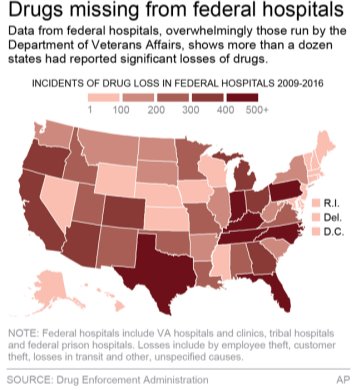
Figure 1. Drug loss from federal hospitals 2009-2016 (Yen, 2017)

Figure 2. Overdose deaths in the United States, by drug, 1999-2016 (Durden, 2017)

Figure 3. Concentration of Overdose Deaths in 2015 (Durden, 2017)

Figure 4. Concentration of Overdose Deaths in 2015 (Durden, 2017)

Figure 5. 2015 opioid-related overdose deaths in Ohio by race and gender (Durden, 2017)

Figure 6. Properties of Urine and hair specimens as analysis media for drug testing (Mieczkowski, 1992)

Figure 7. Chemical substances travel through arteries and are stored in the cuticle cortex (Hair Follicle Drug Testing, n.d.)

Figure 8. Number and type of PDMP agencies in the US (Prescription Drug Monitoring Programs, 2017)

Figure 9. Drug enforcement spending doubled from 2009 to 2016 (Becker, 2017)

Figure 10. Successes of government agencies to reduce CS diversion (Siegel, 2019).
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal



